Application of Bioactive Nano-Glass Fiber in Combination with Fresh Platelet-Rich Plasma on the Re-Epithelialization of the Thermal Wound in Rats
Application of Bioactive Nano-Glass Fiber in Combination with Fresh Platelet-Rich Plasma on the Re-Epithelialization of the Thermal Wound in Rats
Reza Esmaealzade Dizaji1, Arasb Dabbagh Moghaddam1*, Arash Ghalyanchi Langeroudi2, Mohamad Foad Heydari3, Seyyed Javad Hosseini Shokouh4 and Ana Shirzad Shahrivar5
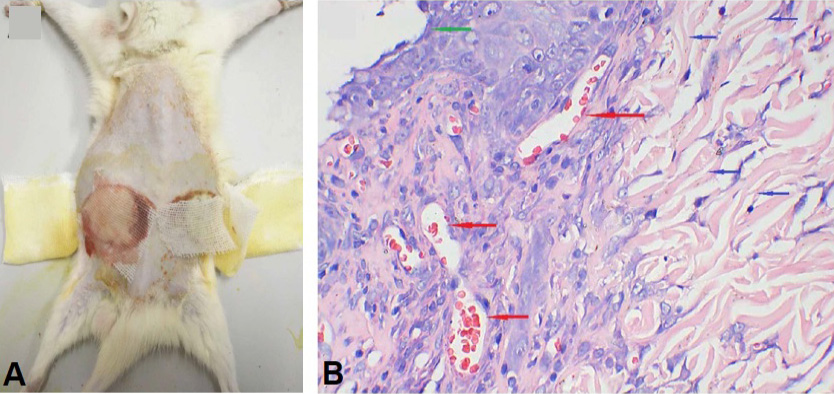
Preparation of deep second-degree scald model and sti pathological evaluation in rat. A: Skin appearance after scald; B: Histopathological properties of skin after scald by H & E staining (×100).
Total decrustation time of the PRP/BNF therapy for deep second-degree scald in rats (n=20, *P<0.05, ***P<0.001, ns: no significance).
A general observation of healing process of deep second-degree scald wounds with a PRP/BNF and PRP therapy in comparison to control groups in rats.
Changes of wound healing rate in rats treated with PRP/BNF for deep second-degree scald (n=5, *P<0.05).
Histopathological changes of deep second-degree scald treated with PRP/BNF by H & E staining (A to L, E=epidermis, G=granulation tissue, ×400); Histopathological score of PRP/BNF for deep second-degree scald wound in rats (n=5, *P<0.05).
Results of qPCR of wound-related genes at different time points on the surface of deep second-degree scalded wounds treated with PRP/BNF in rats (n=5, *P<0.05).