Autologous Platelets-Rich Plasma Gel Promotes Neo-Vascularization and Re-Epithelization in Cutaneous Wound Healing in Rescued Horses
Autologous Platelets-Rich Plasma Gel Promotes Neo-Vascularization and Re-Epithelization in Cutaneous Wound Healing in Rescued Horses
Muhammad Talha Sajjad1, Hamid Akbar1*, Muhammad Arif Khan1, Muhammad Hassan Mushtaq3, Shehla Gul Bokhari1, Muhammad Abid Hayat4 and Ghulam Mustafa2
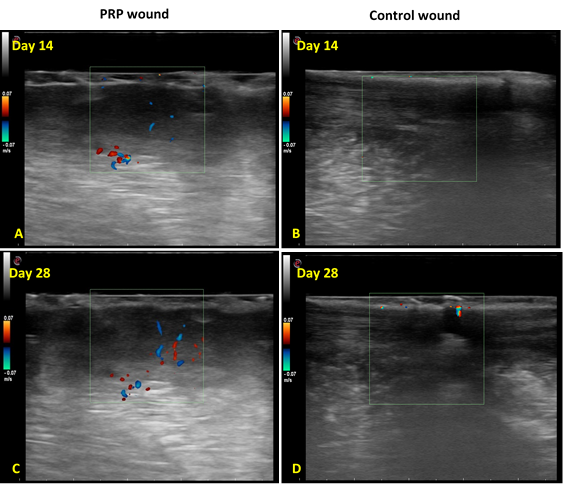
Ultrasonographical evaluation of neo-vascularization in the cutaneous wound of both groups. A; PRP treated wound obtained at day 14 showed mild development of blood vessels. B; Control wound showed no development of neo-vascularization at day 14. C; PRP treated wound at day 28 showed increased development of neo-vascularization at day 28. D; Control wound at day 28 showed mild development of neo-vascularization.
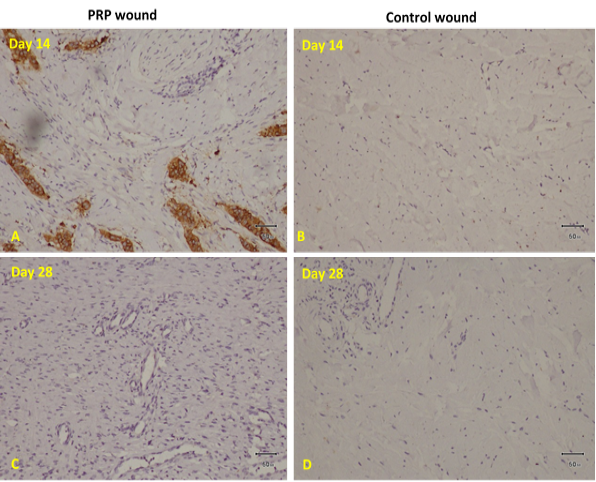
Histopathological evaluation of neo-vascularization in the cutaneous wound of both groups. Bar=50um A, PRP treated wound obtained at day 14 showed mild development of blood vessels. B, Control wound showed no development of neo-vascularization at day 14. C, PRP treated wound at day 28 showed increased development of neo-vascularization at day 28. D, Control wound at day 28 showed mild development of neo-vascularization.
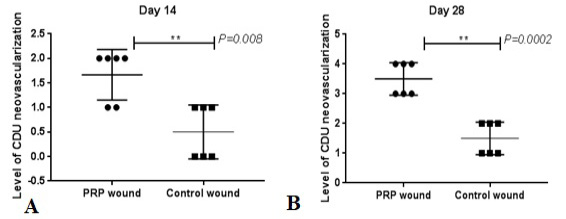
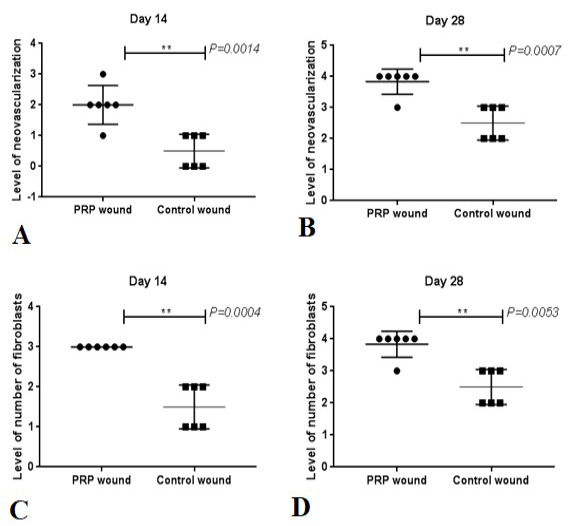
Histopathological scoring of neo-vascularization and fibroblast between the both groups. A, indicates level of neovascularization in PRP and Control wounds at day 14. B, indicates neovascularization in both groups at 28 days. C, indicates level of number of fibroblasts in PRP and Control wounds at day 14. D, indicates level of number of fibroblasts in both groups at 28 days. **, indicated the differences were significant in the PRP-treated group compared with the control group at day 28 (P<0.01).
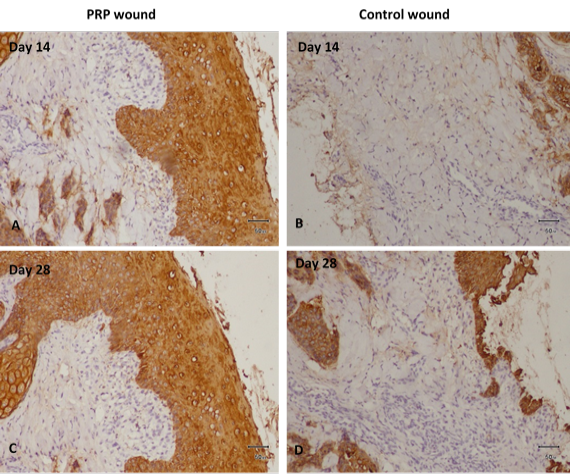
Cytokeratin staining in tissues obtained at Days 14 and 28 after wounding for Re-epithelization in both groups. A, PRP gel treated wound tissue displays accelerated epithelial growth, increased proliferation of connective tissue at day 14. B, Control wound tissue displays no development of epithelial growth, no basal lamina growing, and mild proliferation of connective tissue at day 14. C, PRP gel-treated wound tissue displays increased epidermal growth, intact basal layer, multiple layers of stratum spinosum visible, stratum corneum also visible, and increased fibrous connective tissue on day 28. D, Control wound tissue mild epithelial growth, basal lamina growing, and mild proliferation of connective tissue at 28 days.
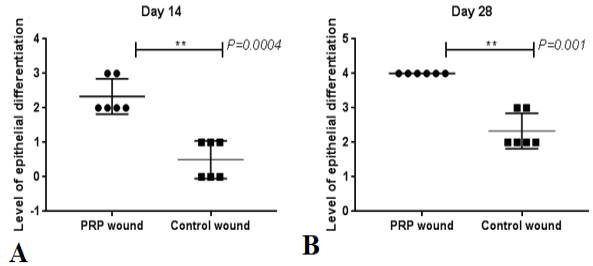
Histopathological scoring of re-epithelization between the both groups. A, indicates level of epithelial differentiation in PRP and Control wounds at day 14. B, indicates level of epithelial differentiation in both groups. ‘**’ indicates the differences were significant in the PRP-treated group compared with the control group at day 28 (P<0.01).